COVID-19: How to Avoid Unexpected Telemedicine Bills

With thanks to advocate and guest blogger, Rob Berman.
Find Rob’s advocacy profile here: Systemedic, Inc Medical Bill Advocate
As COVID-19 (coronavirus) alarmingly spreads throughout the nation, telemedicine is becoming an increasingly common way for doctors to communicate with patients. While the last thing you should be worrying about during this crisis is paying medical bills, high medical expenses may be a real concern if you need to see a medical professional.
If you have symptoms of COVID-19, it’s important to speak with a doctor to determine whether you should get tested. The rules regarding telehealth and coronavirus-related medical treatment are continuing to evolve: although it may appear that coronavirus-related healthcare is fully covered by insurance, there are a few assumptions you should avoid making.
1. Don’t Assume Your COVID-19 Related Telemedicine Visit is Covered by Insurance
Due to COVID-19, telemedicine is used more than ever. Although Medicare used to allow coverage of telemedicine visits only if the recipient lived in a remote area, these requirements have been relaxed. If you are a Medicare patient being evaluated, tested, or treated for Covid-19, you shouldn’t have to pay for a telemedicine visit.
If you have a commercial (private) policy, you can’t assume that your telemedicine visit will be covered. Most insurance companies are waiving cost-sharing and paying the full cost of the visit. In cases where medical insurance does not cover telemedicine, the doctor determines his/her own rates for these non-covered services.
 2. Don’t Assume a Telemedicine Visit NOT Related to COVID-19 is Covered
2. Don’t Assume a Telemedicine Visit NOT Related to COVID-19 is Covered
Since COVID-19 is highly contagious, many doctors are also urging patients to utilize telemedicine for any and all health issues whether or not they are related to COVID-19. Telemedicine visits reduce the risk of being exposed to the virus or exposing others during an office visit.
If you are on Medicare, the costs of a telemedicine visit not related to COVID-19 are covered. However, each commercial insurance company considers telemedicine differently for these types of visits – some companies may apply the cost to your deductible if it hasn’t been met yet. Others are waiving cost-sharing for the duration of the pandemic.
3. Don’t Assume Your Bill is Incorrect If You are Charged a Co-Pay
If you’ve been charged a co-pay for a COVID-19 related telemedicine visit, your bill may or may not be correct, depending on your plan. First, contact the insurance company to find out what your specific plan covers and whether there is cost-sharing you are required to pay. If not, ask your insurance company why they did not pay the claim in full. Depending on their answer, you may need to reach out to your provider to have them correct or resubmit the claim, or request that the insurance company reprocess the claim to reflect the appropriate payment.
4. Don’t Assume Telehealth is Covered Under an Employer-Funded Healthcare Plan
Although most insurance companies are waiving cost-sharing for their fully-funded plans, this may not be the case if your plan is self-funded. A self-funded plan is one in which the employer actually pays for the medical expenses. These employers are typically very large. They hire private insurance companies to administer the plans for them, yet the employers are the ones who fund the payments. If your employer funds the healthcare plan, the same governmental regulations do not apply. Rather, the employer decides how claims will be processed and whether telemedicine is covered at all, with or without cost-sharing.
What Should You Do If You Get an Excessive or High Telemedicine Visit Bill?
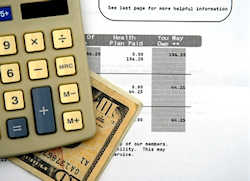
For a telemedicine visit, review the bill for mistakes and inaccuracies as you would any other medical bill. Mistakes in coding and clerical errors can translate into huge expenses.
To determine if your bill is correct:
- Go through the bill line-by-line.
- Make sure your Explanation of Benefits corresponds with the bill.
- Make sure you received the services you are billed for.
In addition, as the coronavirus crisis evolves by the minute, new laws are being enacted every day. It is important to stay informed of any new developments and make sure that you get the benefit of whatever laws apply to your situation.
If you continue to have trouble reconciling your medical bills, whether or not they are related to COVID-19 or telehealth, then tap into the expertise of a medical billing advocate for help.
Find a Health / Patient Advocate or Care Manager
Learn more about The Alliance of Professional Health Advocates
